Earlier this year, news came about the first experimental xenotransplantation: a human patient with heart disease was given a heart from a pig that had been genetically engineered to prevent rejection. While the experiment was initially successful, it ended two months later when the transplant failed, leading to the patient’s death. At the time, the team did not disclose any details about what went wrong. But this week saw the release of a research paper that looks at everything that happened to prepare for the transplant and the weeks after.
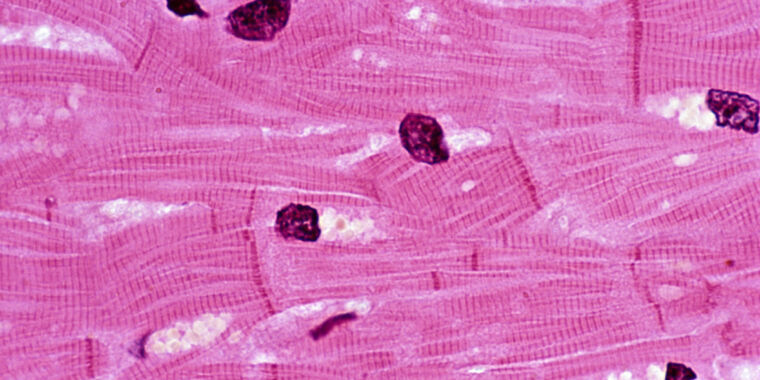
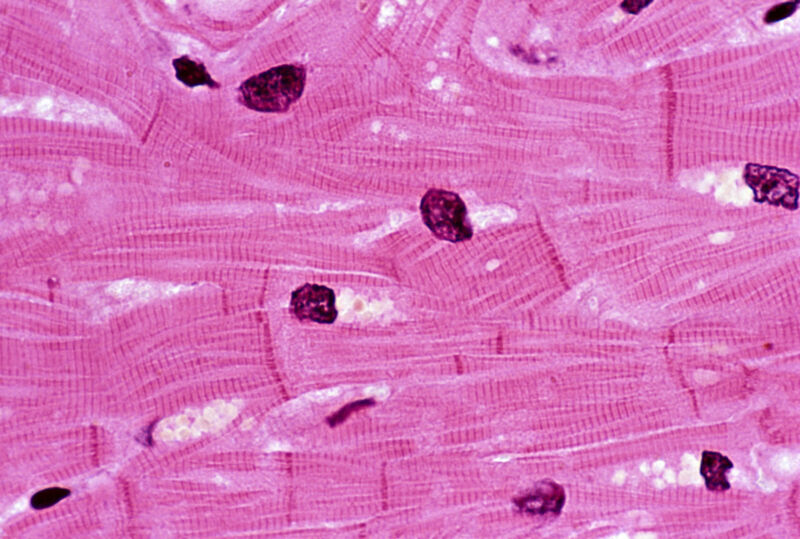
Critically, this includes the eventual failure of the transplant, which was caused by the death of many of the muscle cells in the transplanted heart. But the reason for that death is not clear, and the typical signs of immune system rejection were not present. So we’ll have to wait a little while to understand what went wrong.
A solid start
Overall, the article paints a picture of organ recipient David Bennett as a patient about to die when the transplant happened. He was an obvious candidate for a heart transplant and was kept alive only through the use of a device that helped oxygenate his blood outside of his body. But the patient had what the researchers call “poor adherence,” which led to four different transplant programs denying him a human heart transplant. At that point, he and his family agreed to participate in the experimental xenotransplantation program.
The pig that served as a heart donor came from a population that has been extensively genetically engineered to limit the possibility of rejection by the human immune system. The line was also free of a specific virus that inserts itself into the pig genome (endogenous retrovirus C or PERV-C) and was grown under conditions that should limit exposure to pathogens. The animal was also screened for viruses prior to transplantation and the patient was then screened for swine pathogens.
After the transplant, the patient’s new heart performed well, with a normal rhythm between 70 and 90 beats per minute. Most significantly, more than half of the blood filling the left ventricle of the transplanted heart was sent to the circulation with each contraction; that was a mere 10 percent increase in the diseased heart it had replaced.
About two weeks after the transplant, Bennett started experiencing abdominal pain and weight loss, which eventually led to him losing more than 20 kg (40 lbs). He was placed on a feeding tube and an exploratory laparoscopy showed possible signs of an infection that was clearing, but no action was considered necessary. Moments later, screening revealed a possible infection with the porcine version of the cytomegalovirus; the human version of this virus causes problems such as pneumonia and mononucleosis. This was treated with antiviral treatments.
Although weight loss was an obvious concern, five weeks after the transplant, there was no evidence of rejection and the heart was still functioning.