James Kirkland began his career in 1982 as a geriatrician, treating aging patients. But he found himself dissatisfied with what he could offer them.
“I got tired of being prescribed wheelchairs, walkers, and incontinence pads,” recalls Kirkland, now at the Mayo Clinic in Rochester, Minnesota. He knew that aging is considered the biggest risk factor for chronic disease, but he was frustrated by his inability to do anything about it. So Kirkland went back to school to learn the skills he needed to tackle aging head-on, earning a PhD in biochemistry from the University of Toronto. Today, he and his colleague Tamara Tchkonia, a molecular biologist at the Mayo Clinic, are leaders in a growing movement to halt chronic disease by protecting brains and bodies from the biological effects of aging.
If these researchers are successful, they will have no shortage of clients: People are living longer and the number of Americans aged 65 and older is expected to double to 80 million by 2040. While researchers like Kirkland don’t expect to extend lifespan, they hope to extend the “health period extend the time a person lives free of disease.
One of their targets is decrepit cells that accumulate in tissues as people age. These “senescent” cells have reached a point — from damage, stress, or simply time — where they stop dividing, but don’t die. While senescent cells typically make up only a small fraction of the total cell population, they accounted for up to 36 percent of cells in some organs of aging mice, one study showed. And they don’t just sit there quietly. Senescent cells can release a slew of compounds that create a toxic, inflamed environment that prepares tissues for chronic disease. Senescent cells have been linked to diabetes, stroke, osteoporosis and several other aging conditions.
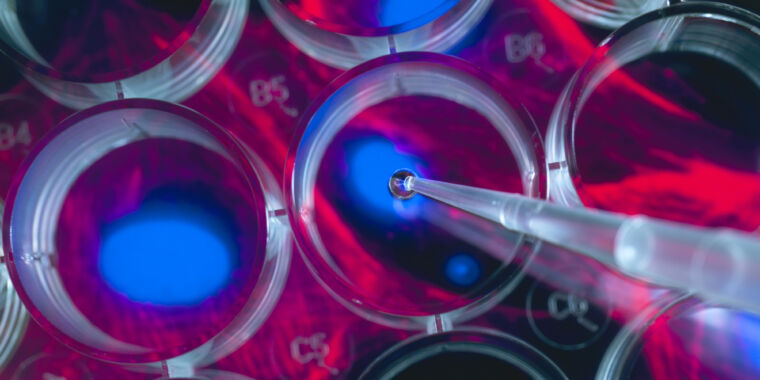
These harmful cells, along with the idea that removing them could reduce chronic disease and the discomforts of aging, are getting serious attention. The U.S. National Institutes of Health is investing $125 million in a new research effort called SenNet, which aims to identify and map senescent cells in the human body and in mice throughout the natural lifespan. And the National Institute on Aging has raised more than $3 million in four years for the Translational Geroscience Network’s multicenter team led by Kirkland, conducting preliminary clinical trials of potential anti-aging treatments. Drugs that kill senescent cells — called senolytics — are among the top candidates. Small-scale trials are already underway in people with conditions such as Alzheimer’s, osteoarthritis and kidney disease.
“It’s an emerging and incredibly exciting, if not groundbreaking field,” said John Varga, chief of rheumatology at the University of Michigan Medical School in Ann Arbor, who is not part of the TGN.
But he and others also warn, and some scientists think the field’s potential is overstated. “There’s a lot of hype,” says Varga. “I have, I would say, a very healthy skepticism.” He warns his patients about the many unknown factors and tells them that trying senolytic supplementation on their own can be dangerous.
Researchers are still unraveling the biology of senescent cells, not only in aging animals but also in younger ones – even in embryos, where the aging of certain cells is crucial for proper development. So far, evidence that destroying senescent cells helps to improve health spans has mostly come from laboratory mice. Only a few preliminary human trials have been completed, with hints of promise but far from blockbuster results.
Still, Kirkland and Tchkonia speculate that senolytics may ultimately help not only with aging, but also with conditions that younger people suffer from injury or medical treatments such as chemotherapy. “Maybe there are applications everywhere,” Kirkland muses.