Researchers in the UK have come up with the most detailed, complex hypothesis yet to explain the outbreak of mysterious cases of liver inflammation – also known as hepatitis – in young children, which has been troubling medical experts worldwide for several months.
The cases first came to light in April, when doctors noticed an unusual cluster of hepatitis cases in young children in Scotland. The diseases were not linked to a known cause of hepatitis, such as hepatitis (A to E) viruses, making them unexplained. While unexplained cases of pediatric hepatitis do occur from time to time, a report that month listed 13 cases in Scotland in two months, while the country would typically see fewer than four a year.
Since then, the World Health Organization has counted more than 1,000 possible cases from 35 countries. Of those cases, 46 required liver transplants and 22 died. The Centers for Disease Control and Prevention identified 355 cases in the US. As of June 22, 20 cases in the US required liver transplants and 11 died.
Hypotheses to explain the cases were broad. Some have suggested – notably adamantly – that the cases may be aftereffects of infection with the pandemic coronavirus, SARS-CoV-2. The CDC, meanwhile, released data showing that there has been no increase in pediatric hepatitis cases or liver transplants from pre-pandemic baseline levels, suggesting that the unusual clusters may not represent a new phenomenon.
Combination of factors
But a common feature of the cases was infection with an adenovirus. The extremely common childhood viruses have surfaced in many cases. As such, many hypotheses relate to adenoviruses, but this too is puzzling, because adenoviruses not known to cause hepatitis in previously healthy children.
In two new reports, British researchers offer a new hypothesis that may be the clearest but most complex explanation. Their data suggests that the cases may result from a co-infection of two different viruses — one of which may be an adenovirus and the other a hitchhiking virus — in children who also happen to have a specific genetic predisposition to hepatitis.
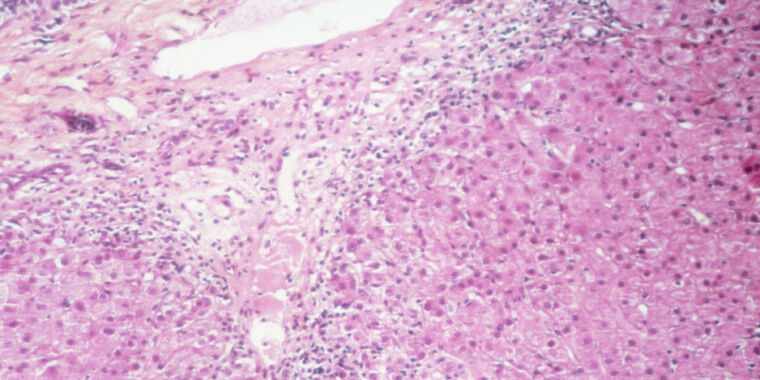
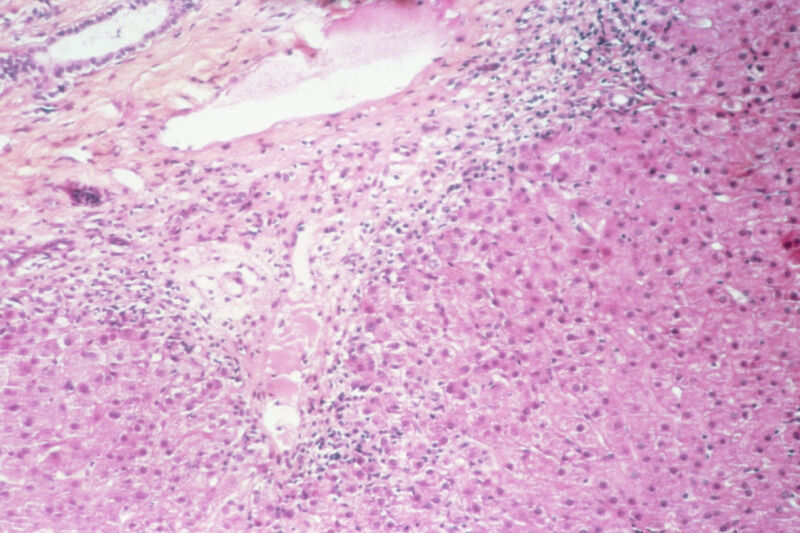
In one of the new studies, looking at nine early cases in Scotland, researchers found that all nine children were infected with adeno-associated virus 2 (AAV2). This is a small, non-enveloped DNA virus in the Dependoparvovirus sex. It can only multiply in the presence of another virus, often an adenovirus but also some herpes viruses. As such, it tends to travel with adenovirus infections, which peaked in Scotland when the puzzling cases of hepatitis occurred.
Most notably, although all nine hepatitis cluster cases were positive for AAV2, the virus was completely absent in three separate control groups. It was found in zero of 13 healthy control children of the same age; zero of 12 children who had an adenovirus infection but normal liver function; and zero of 33 children who were hospitalized with hepatitis for other reasons.
This finding was supported in a separate study led by researchers in London, which examined 26 unexplained cases of hepatitis with 136 controls. It also found AAV2 in many of the hepatitis cases, but in very few of the control cases.
aptitude
The study of the nine cases in Scotland went a step further by examining the genetics of the children. The researchers noted that eight of the nine children (89 percent) had a gene variant for a human leukocyte antigen called HLA-DRB1*04:01. But this gene variant is only found in about 16 percent of Scottish blood donors, well below the frequency found in the cases of hepatitis. In addition, HLA-DRB1*04:01 is already known to be associated with autoimmune hepatitis and some cases of rheumatoid arthritis.
In general, human leukocyte antigen (HLA), also known as major histocompatibility complex or (MHC), are proteins outside of immune cells that present antigen – such as viral or bacterial peptides – to T cells. This presentation teaches the T cells how to respond to potential threats, elicit immune responses to invading germs or tolerance to specific antigens. HLA proteins thus play a critical role in influencing immune responses.
The Scottish study suggests that all three factors together explain the hepatitis cases: an adenovirus infection and a tag-along AAV2 infection, one of which triggers an aberrant immune response in genetically predisposed children. It is unclear how exactly all the factors combine, but based on the nine cases, all three factors are necessary. This could explain why hepatitis cases are so rare, linked to adenovirus infections, and appeared to cluster after pandemic restrictions were lifted, when many susceptible children became infected with common viruses, including adenoviruses.
Of course, this is just a hypothesis for now — and one based primarily on just nine cases in a study yet to be peer-reviewed. Researchers will need to do much more work to determine whether this hypothesis explains the cases, including looking at larger cohorts of children and molecular research to understand the potential mechanism.