An existing vaccine that prevents meningococcal disease may also be up to 40 percent effective at preventing gonorrhea infections, which are becoming increasingly resistant to antibiotics, with some strains being completely incurable. This discovery is according to a series of studies and commentary published Tuesday in The Lancet Infectious Diseases.
While estimated effectiveness is modest, injections of the vaccine — 4CMenB aka Bexsero — can still prevent many infections, researchers reported. The vaccine could prevent more than 100,000 gonorrhea infections in the UK in 10 years, saving an estimated $10.4 million. In the meantime, the vaccine’s effectiveness could provide important clues for vaccine developers to create a more effective gonorrhea-specific injection.
The need for such a vaccine is clear. Not only is gonorrhea rapidly becoming more drug-resistant, but it is also increasing in the US and other countries. The World Health Organization estimates that there were more than 82 million cases of gonorrhea worldwide in 2020. The U.S. Centers for Disease Control and Prevention estimate that there were nearly 680,000 cases in the U.S. in 2020, a 10 percent increase from 2019 and a 45 percent increase from 2016.
In a news conference Tuesday, Jonathan Mermin, director of the CDC’s National Center for HIV, Viral Hepatitis, STD and TB Prevention, emphasized the optimism surrounding using 4CMenB to prevent gonorrhea. “More research is being done on that,” Mermin noted, “but it shows at least some hope that we could develop effective and safe vaccines against gonorrhea in the future, which would help us more successfully reverse some of the trends.” return we”ve seen in the last ten years.”
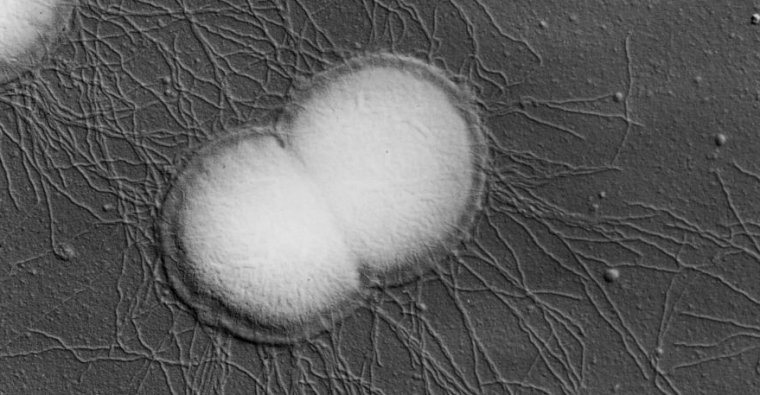
The effectiveness of a meningococcal vaccine against gonorrhea stems from the fact that the two diseases are caused by related bacteria — Neisseria meningitidis and Neisseria gonorrhoeae, respectively. Previous research has suggested that the vaccine could provide cross-reactive immune responses, as the two microbes share significant amounts of their genetic code and key proteins targeted by the vaccines.
Multifunctional vaccine
In the series of studies published Tuesday, there were two case-controlled observational studies examining the true effectiveness of 4CMenB against gonorrhea infections in specific populations in the US and Australia.
In the US-based study, led by Winston Abara of the CDC, researchers used health records of cases of gonorrhea in people ages 16 to 23 in New York City and Philadelphia from 2016 to 2018. had chlamydia – the control group.
The researchers had records of nearly 168,000 infections (about 18,000 gonorrhea infections, 125,000 chlamydia infections and 25,000 co-infections) among nearly 110,000 teens and young adults. Of those, nearly 7,700 had been vaccinated with at least one dose — about 4,000 had one dose and 3,600 had two doses. The researchers estimated that having two doses provided 40 percent protection against gonorrhea, and one dose was 26 percent effective.
In the second study, Australian researchers used data from more than 53,000 teens and young adults who received one dose and 46,000 who received two doses in South Australia as part of a statewide program. Looking at the vaccination status of gonorrhea cases and using chlamydia cases as controls, the researchers estimated that the 4CMenB vaccine was 33 percent effective in preventing gonorrhea.
The studies have several limitations. For example, the researchers cannot determine how long such protection against gonorrhea can last after vaccination. The studies looked at specific populations, so the estimates may not be generalizable. Still, any modest benefits could significantly influence the spread of the disease, especially in high-risk groups, such as young adults and men-who-sex-with-men (MSM).
In a third study released Tuesday, researchers in the UK modeled the cost-effectiveness of using the meningococcal vaccine 4CMenB to prevent gonorrhea infections. They estimate that vaccinating high-risk MSM could prevent 110,000 cases in the UK over the next 10 years, saving $10.4 million in testing and treatment costs. And those estimates are conservative. The researchers assumed that one dose of the vaccine offers no protection. The study also did not account for additional costs that may be associated with drug-resistant gonorrhea infections.
“With a gonorrhea-specific vaccine likely to take years to develop, an important question for policymakers is whether the meningitis vaccine 4CMenB should be used against gonorrhea infection,” said lead author of the pilot study, Peter White, of Imperial College London in a statement. “Our analysis suggests that giving the vaccine to those at greatest risk of infection is the most cost-effective way to prevent large numbers of cases.”

